Blood glucose meter purchasing advice: how to choose the right product
- What you need to know
- Blood glucose meters, or glucometers, measure the sugar levels in your blood.
- Most glucose meters need a pinprick of your blood to work.
- Infrared glucose meters work without needing to prick your skin, CGM meters use a sensor implanted under your skin.
- Blood glucose meters are an effective way for people with diabetes to manage their condition from day to day.
Put control in your own hands
Diabetes is a metabolic disorder that affects more than 400 million people worldwide. It is characterized by high blood sugar levels. To effectively manage diabetes, you need to regularly check your blood sugar levels. Blood glucose meters allow you to do this, and they only take a few seconds to give you the results. Doctors can then use this data to help adjust your medication.
Blood sugar refers to the amount of glucose in your blood. Our bodies use glucose as an energy source. It is absorbed into your blood during digestion in your intestine. Insulin is the hormone responsible for regulating the transport of glucose into the cells in which it is used. In other words, it is responsible for our blood sugar levels. If you have diabetes, your body does not produce or respond to insulin properly, which causes changes in your blood sugar level.
Typical symptoms of diabetes include increased urination frequency, tiredness, poor concentration, problems with vision, itching, severe thirst, and cravings. Uncontrolled diabetes is dangerous as it makes the body vulnerable to disease. Diabetes also increases the risk of developing high blood pressure which can damage your eyes, nervous system, and heart.

It is extremely important for diabetes patients to be able to regularly measure their blood sugar levels, as it can help control diabetes. Blood glucose meters make this easy. All you need to do is put a pinprick of blood onto a test strip, and the machine will quickly produce the analysis.
Type 1, type 2, and gestational diabetes
There are three main types of diabetes: type 1, type 2, and gestational diabetes. Type 1 diabetes is an autoimmune disease and can often occur at a young age. In type 1 diabetes, the body’s immune system attacks the insulin-producing beta cells in the pancreas. This means that the body doesn’t have enough insulin, which results in high blood sugar levels. Insulin deficiency is a lifelong condition, and patients need to regularly inject insulin to keep their blood sugar under control. At the moment, the causes of type 1 diabetes are not completely clear, but many scientists hypothesize that it is genetic.
Type 2 diabetes is the most common form of diabetes. It is not caused by insulin deficiency, but instead by insulin resistance. This means that the cells in the body don’t react properly to insulin, causing blood sugar levels to rise. In response to this, the pancreas produces increased amounts of insulin, which eventually damages it to the point that it can no longer produce enough insulin. At this stage of the condition, patients need to inject insulin to combat the deficiency.
Gestational diabetes may be developed by pregnant women. Even without having had type 1 or 2 diabetes prior to the pregnancy, it is possible to occur, although the high blood sugar levels usually return to normal after birth. There is then, however, a higher risk to develop type 2 diabetes later.
Blood sugar
The concentration of sugar in your blood depends on what you have eaten. When using a blood glucose meter, you need to know what the numbers mean when you get them back. Confusion can sometimes occur due to different units of measurement:
- Millimoles per liter (mmol/l)
- Milligrams per deciliter (mg/dl)
Millimoles per liter (mmol/l) indicates the quantity of sugar molecules per liter of blood. Milligrams per deciliter (mg/dl) describes the weight of the sugar molecules in one deciliter of blood. Both units of measurement are common on blood glucose meters, so make sure you know which one you are dealing with.
The following table gives the range for normal blood sugar levels. The values are different depending on whether you have an empty stomach (at least 8 hours since eating) or if you have just eaten. These two states are often referred to as preprandial (before a meal) and postprandial (after a meal).
| Normal value in mg/dl | Normal value in mmol/L | |
| Preprandial | 60–100 mg/dl | 3.3–5.5 mmol/L |
| Postprandial | 90–140 mg/dl | 5.0–7.8 mmol/L |
How do blood glucose meters work?
Most meters work using a pinprick drop of blood. Most devices are smaller than a smartphone, which means they are easy to carry around. They come with a lancet and a lancing device, as well as test strips. A lancet is a small blade with a plastic handle which you use to prick your skin. Lancing devices are spring loaded to make drawing blood easier. To test your blood, you just have to put a drop on the test strip.
Types of blood glucose meter
There are three main types of home blood glucose meters: standard, continuous, and infrared. Standard devices work using a pinprick sample of blood. Continuous glucose meters use sensors under your skin to measure the glucose in your fatty tissue. Infrared meters don’t need a sample or sensors, you just put your finger on an IR sensor. These are the latest in blood glucometer technology, but their efficacy and accuracy is not 100% reliable.
Standard blood glucose meters
Blood glucose meters that use a blood sample are widely used. They can be used multiple times a day, and only need an extremely small drop of blood to work. The droplet goes on a test strip, which you then put into the glucometer to get the reading. When used properly, this type of blood glucose meter will give an accurate analysis of your blood sugar level.
Standard glucose meters tend to come in two different styles:
Single-use strip meters need a new test strip for each analysis. They are easy to use, but you need all the accessories: test strips, lancets, and lancing devices.

Integrated meters are an all-in-one solution. The test strips are in a roll which is inside the meter. They also have integrated lancets. While these meters are larger than single-use strip meters, they aren’t too big, so they are still quite easy to transport
Continuous blood glucose (CGM) meters
Continuous blood glucose monitoring, or CGM, is a noninvasive method of measuring blood sugar. Instead of using a drop of blood, these devices measure the glucose content in the fatty tissue under your skin. To use one of these meters, you need to have a sensor implanted under your skin. Most of the time, these need to be changed every 5 to 14 days, but you can get sensors implanted by healthcare specialists that last up to six months. The sensor automatically transfers your blood sugar levels to a connected meter. This lets you monitor your blood sugar in real time — especially useful if you need to check your levels frequently.
Infrared meters (noninvasive)
Infrared glucometers are the latest in blood sugar analysis technology. They are noninvasive, which means that all you need to do is put your finger on an infrared sensor — nothing pierces your skin. These meters are still in development, and as such are not considered completely accurate or reliable because there aren’t any reliable long-term scientific studies on them yet.
Purchasing tips
When choosing a blood glucose meter, there are a few things you need to consider. These factors are mainly to do with ease and frequency of use. The bottom line is you want the best type of meter for your needs, that is reliable and fast.
Accuracy
An inaccurate blood glucose meter is useless. In other words, accuracy is the most important factor when it comes to glucometers. There are various accuracy deviation standards from national and international medical bodies to ensure that blood glucose meters are precise. For example in the EU, blood glucose meters need to follow the ISO standard 15187:215. It states that, if the blood sugar value is below 100 milligrams per deciliter (5.5 millimoles per liter), 95% of the measured values may be within a fluctuation range of plus or minus 15 milligrams per deciliter (1.8 millimoles per liter). If the blood sugar value is over 100 milligrams per deciliter, a deviation of no more than 15% is permitted.
Most manufacturers publish information on the accuracy and deviation limits of their meters. These can usually be found online and in the manual. If you are unsure about your meter, get your doctor to do a measurement so you can compare the precision of your device.
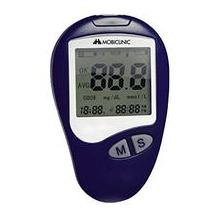
Operation and display
Blood glucose meters are designed to make life easier, not more difficult. They should be simple to use to prevent any false measurements. Likewise, they should have a clear, readable display — pictograms and labels are a useful feature in this regard. The display should be large and backlit so you can use it in all lighting conditions.
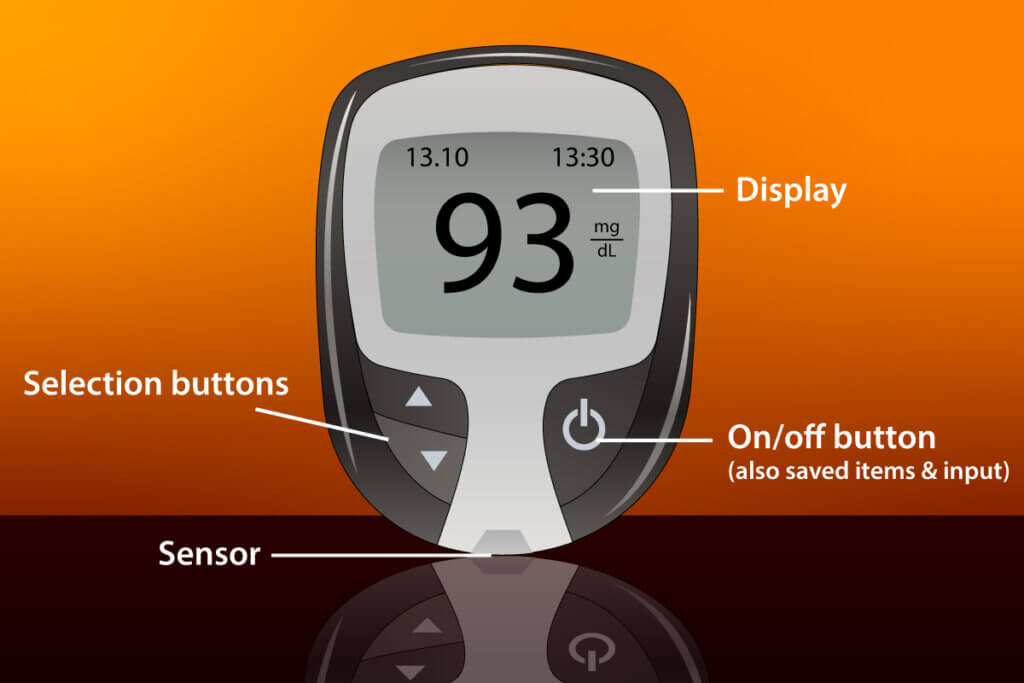
Most glucose meters have similar designs. The measurement result (or an error code in the event of an incorrect measurement) is usually given in the middle of the display. Above are the date and time. An apple stands for a measurement before a meal (preprandial), while an apple core symbolizes a measurement after eating (postprandial). Most devices have a diary feature, which lets you look back over the recent readings — this is often indicated by a book symbol. Meters usually have selection buttons and a confirmation button, which can also be used to switch the meter on and off.
Measuring time
For many diabetics, the speed with which their blood glucose meter gives a reading plays an important role. Getting a fast reading is particularly crucial in emergencies. Single-use strip meters will give you your results a few seconds after inserting the test strip.
If you have a CGM meter, analysis speed is less important, as the meter will take readings at regular intervals which you can evaluate later.
Size and weight
Dimensions are important as you will want to bring your blood glucose meter with you in your day to day life. Most meters aren’t much bigger than a mobile phone and weigh between one and two ounces (30-50g). While integrated meters are often an easier option (as you don’t need to remember any accessories), they are a little heavier than single-use strip meters.
Storage space
Being able to save blood sugar level measurements makes treating diabetes easier, as it lets you analyze changes over time. Storage is therefore an important criterion when it comes to choosing a blood glucose meter. A good meter should let you store up to 500 measurements.
Some meters have a USB interface which lets you transfer your readings to a computer or smartphone, so you can keep an electronic diabetes diary. A lot of manufacturers also offer apps to help with this.
Coding
Many meters on the market nowadays need to be ‘coded’. This means they need to be calibrated to work with new test strips. If your meter needs to be manually coded, it means you need to input the number on the test strip pack.
Automatic coding makes using a meter easier, more time-efficient, and safer. As soon as you put a new test strip in, a meter with automatic coding will recognize it and adjust the settings.
Extra features
The sections above cover the essentials when it comes to blood glucose meters, but there are a few non-essential extras you might want to consider when choosing a device.
A lot of meters have an alarm which will let you know when you need to make a measurement.
Some meters let you take blood samples from different parts of your body, not just your finger tip. These are known as AST (Alternate Site Testing) meters.
Most meters will come with a USB cable so you can transfer your measurement diary. However, some meters are also Bluetooth or Wi-Fi enabled, so you can make a wireless transfer.
Usage tips
After a while regularly measuring your blood sugar levels, using a blood glucometer will become routine. If you’re just starting out though, here are some useful tips.

Common mistakes
It is essential that you are getting accurate readings from your blood glucose meter. When first using your meter, make sure you get proper training from your doctor.
One common mistake is leaving your test strip jar open. This can allow too much moisture to get in, which can invalidate the strips. It is best practice to close the jar immediately after removing a strip.
If you get blood on a strip before putting it in the meter, it will invalidate your results. Most meters only ask for a blood sample after you have correctly inserted a test strip.
When taking a blood sample, avoid getting it from your thumb or index finger. These are the most used fingers in daily life. Most people take blood from their ring finger.
Don’t try to squeeze out a drop blood. This causes cell fluid to come out of your finger, which can invalidate the reading.
When collecting blood, your finger needs to touch the side of the test strip so it can absorb the blood properly. Don’t hold your finger on the strip from above, as this can prevent the blood from reaching the measurement zone.
Recognizing errors
A lot of modern blood glucose meters are error sensitive. This means that they will recognize when the meter hasn’t been used properly and the measurement is inaccurate. Depending on the model, some meters can specify what the error is.
Improving your blood sugar levels
Nowadays, diabetes is a very treatable disease. As well as regularly self-monitoring and taking insulin, those affected also have other avenues for improving their health. Diet and exercise play an extremely important role in the treatment of type 2 diabetes. However, these tips are also helpful for patients with type 1 diabetes.
A balanced and healthy diet is good for everyone, no matter your health. Overweight patients should try to reduce their weight slowly. Changing your eating habits is the most effective, long-term way of achieving this. Lots of fiber, fresh fruit, vegetables, and whole grain products make up a balanced diet.
Everyone, diabetics included, should make sure to drink enough fluids. At least half a gallon (2L) per day is recommended. Ideally, this should be water or other unsweetened drinks. Diabetic patients should only drink alcohol on rare occasions, if at all.
Exercise is also very important. The aim is not to become a competitive athlete: regular cycling, swimming, or even just going for a walk is often enough. Small changes in habits can have a large effect. Leave the car and walk or climb the stairs instead of taking the elevator.
Sleep disorders and lack of sleep have a negative effect on insulin release and blood sugar levels. It’s important that you get enough sleep. Also remember to take small breaks every day.
Smoking harms the body in many ways. It is believed that nicotine and other substances found in cigarettes have a harmful effect on insulin production.
Image 1: © FinalCheck | Image 2: © Goffkein / stock.adobe.com | Image 3: © Jürgen Fälchle / stock.adobe.com | Image 4: © FinalCheck | Image 5: © Mike / stock.adobe.com













 5,672 reviews
5,672 reviews






